How we support carers
Triangle of Care 
The Triangle of Care is a self-assessment tool for service providers developed by the Carers’ Trust. It’s based on the principle that care is improved by having good working relationships between the service user, the mental health professional and the carer.
It helps services think about how they can engage and support carers more effectively, and promote a ‘carer aware’ culture on our hospital wards and in our teams.
Dorset HealthCare is committed to the Triangle of Care, and has cemented that commitment by signing up to its audit process. This means the Carers’ Trust will monitor our progress in implementing these key elements:
- Carers and the essential role they play are identified at first contact or as soon as possible thereafter.
- Staff are ’carer aware’ and trained in carer engagement strategies.
- Policy and practice protocols re: confidentiality and sharing information are in place.
- Defined post(s) responsible for carers are in place.
- A carer introduction to the service and staff is available, with a relevant range of information across the acute care pathway.
- A range of carer support services is available.
This is a joint initiative between the Trust's and is delivered in partnership Dorset Mental Health Forum, Rethink and Dorset Mental Health Carers Project.



As part of the accreditation all staff will have had carer awareness training delivered in partnership with lived experience.
Here Joy and Trish talk about their involvement in the Triangle of Care.
 Expert by Experience / Carer Peer Specialist
Expert by Experience / Carer Peer Specialist
Joy Ford was a carer to my son, and now a part time supporter to my daughter who has an eating disorder and a full time carer to my husband.
The Triangle of Care was launched in Dorset in 2016, at that time there were large meetings of on patient staff attending learning set that were co-produced with medical staff and carer. That co-production has continued over the years, but the training has been evolving over this time. During lock down we went from going in person to a ward or a CMHT service to give a presentation, to working on Teams.
With Pat Wilkins (Carers Development Lead), Trish McLennan (expert by experience) and myself, we have tweaked the presentation, and shortened it over time to not only keep it up to date as things change, but each presentation can bring up a question or thought from the staff attending, that helps us to improve, and keep it on trend.
Over my time of being involved with the TOC I have seen the way things have changed for the family and carers. Staff are far more aware of the knowledge a carer carries about the patient, and how they may help. Also speaking to carers many feel listened to more and valued by staff, they are sign posted to farther help and support even in these difficult times.
There are small pockets where something may go wrong but we are all human. There are many resources on the Net now, including podcasts and webinars and videos, all to help bring an understanding for carers and staff. Working together brings the best out for all of us.
 Trish McLennan Expert by Experience
Trish McLennan Expert by Experience
I have my own “lived experience” of being a carer for my late husband and son.
I have been involved in co presenting the carers awareness training for over a year along with Pat and Joy.
Over this period, we have tweaked the presentation several times.
My own lived experience is quite open, and I have recently updated my input to include an example of “what made a difference” during my caring years.
Within the breakouts rooms we have had a very varied range of discussions and within the question section it allows staff the space to ask questions to other staff, for example “what you would have done in this situation.
The training also has a section of organisations that carers can be signposted to, by the relevant staff.
I do think personally that the training is an excellent training tool within a person’s development, and it also gives staff a valuable insight into some of the difficulties that carers face by Joy and I speaking openly about our own “lived experience “.
The carers awareness training is well attended, and we do receive very positive feedback back from the attendees.
Examples being
- It’s made me realise how important carers are
- Look at the bigger picture
- Grateful to hear things from a carer’s perspective
- Insightful / informative
For more information please email dhc.triangleofcare@nhs.net
Getting carers feedback is so important for two reasons
- how we can look at improving our services
- sharing really good practice that can be shared back with the teams
Its has now been made easier:
Through the internet link below
https://gthr.co.uk/15e8 (easy read)
You can read more about the Triangle of Care at the Carers’ Trust https://carers.org/resources/all-resources/53-the-triangle-of-care-carers-included-a-guide-to-best-practice-in-mental-health-care-in-england
Brief on Triangle of Care
The triangle of care is a model Dorset HealthCare has decided to adopt across the trust.
This is done in three stages and each stage is submitted to the Carers Trust who will award the stars/ accreditation.
Process of Triangle of Care
Stage 1: Inpatient and Crisis Services
Stage 2: CMHTs and CAMHS
Stage 3: Community Services
The stages involve completing a self-assessment and updating this yearly. This is RAG rated by the team, red, amber or green.
Self-Assessment
Four Key Stages:
Ø Complete Self-Assessment
Ø Collate Evidence for each section
Ø Develop Team action plan to develop Amber and Red areas
Ø Review self-assessment and develop action plans
We have been awarded our first and second star and now working with our community hospitals to submit stage 3 by February 2023 to gain our third star.

Over the last five years we have worked with 67 teams who have a carer lead (this role is to ensure the team are carer aware and work together when it comes to carers) they have all had carer awareness training in partnership with our carer peer specialists.
We have learning sets every quarter for carer leads to attend and this is a time to reflect where they are and give any national updates. We always have at least 55 people attend each time.
There is a steering group that meets quarterly and the membership is made up of carer leads, carer peer specialist Phil Morgan (Lead for Recovery and Social Inclusion) and Pat Wilkins(Carers Development Lead).
In our last CQC inspection it was the Triangle of Care was highlighted as good practice.
Carer's Passport in our Hospitals
Hospitals across Dorset recognise the vital role that carers play in the health and wellbeing of those they care for.
Hospital staff recognise that carers are often the experts in their cared-for person’s care and want to support and work with carers to ensure a smooth patient and carer experience in hospital.
Dorset County Hospital, Dorset Healthcare NHS Foundation Trust and University Hospitals Dorset NHS Foundation Trust have come together, with the support of local carers and other carer professionals, to create an ‘Our Dorset’ Hospital Carer Passport, as apposed to the current scheme we have in place currently.
Dorset HealthCare will start with Shaftsbury and Sherbourne community hospitals and role it out across our other community hospitals at a later date. Our current carers passport will still be used until the change over.
The aim is to help carers be recognised and supported with their stay in hospital.
The purpose of the Carer Passport is to clearly identify carers when their cared-for person is admitted into hospital and for staff to welcome, involve and support carers while also helping them to understand the needs of the cared-for person throughout their hospital stay.
Carers have a right, but not a duty, to continue to care while their cared-for person is in hospital.
The Carer Passport scheme includes*:
· Flexibility with visiting times 
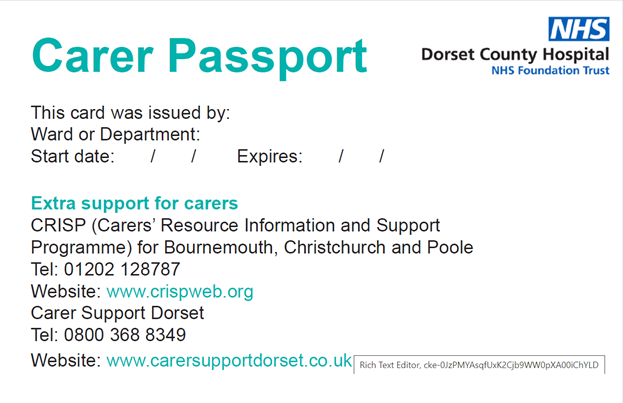
· Inclusion in care
· Inclusion to assist at mealtimes
· Involvement in discussing and planning for discharge
· Access to information about patient care (with relevant consent)
*Each hospital’s passport offer may differ.
The benefit of a Hospital Carer Passport encourages hospital staff to have ‘carer conversations’ to ensure carers are involved and supported in their cared-for person’s care from admission through to discharge. For this reason, Carer Passports are non-transferrable from hospital to hospital.
“Communication is the key challenge to face, or rather lack of communication. Getting the message across to the medical specialists about the particular needs and wants of the patient’s medical needs is so important. We need staff to realise every patient is individual and no one has all the answers, but they can listen to us as a carer. I’m not a medical professional but I am a reasonable expert in my own wife…” Mark, carer
For further information please contact:
Dorset County Hospital (Dorchester): https://vimeo.com/727710862 password is MeghanG
Tel: 0800 7838058 (Patient Experience Team) Email: pals@dchft.nhs.uk
Dorset Healthcare NHS Foundation Trust
Tel: 01202 443261 (Participation Team)
https://www.dorsethealthcare.nhs.uk/contact-us
University Hospitals Dorset NHS Foundation Trust (Bournemouth, Christchurch, Poole)
Tel: 0300 019 8714 (Carer Support Service) Email: carersupport@uhd.nhs.uk

Knowing who the carer is for our patients is so important as they know their loved ones best , as staff we always put the patient at the centre of all that we do, it is crucial that we work with carers to understand the individual needs of our patients so that we can provide the best care possible enabling them to reach full potential. Utilising the carers passport on the ward shows patients and their carers that we value their knowledge and experience and want to work with them throughout their admission and subsequent discharge, recognising what matters most to them. The carers passport enables carers to be fully involved in all aspects of the patients journey from the beginning, it helps staff have a greater understanding of that patients individual needs .
Ali Low
Matron
Westminster Memorial Hospital/Yeatman Hospital
