The Brain Health Clinic
We currently have a varied portfolio of research studies taking place. Each study differs in what is required from a participant. Please read the summaries below to find out more or email us at dhc.
UK-EDI: UK Early Detection Initiative for Pancreatic Cancer
Specialty area: diabetes and cancer
The UK-EDI study aims to improve detection of pancreatic cancer in high-risk groups, using a variety of different methods. Most cases of new-onset diabetes are due to lifestyle or genetic factors, but in a small subset of people diagnosed with new onset diabetes the diagnosis is believed to be an early sign associated with the development of pancreatic cancer.
Who can take part in the study?
People aged 50 or more who have received a diagnosis of diabetes within the last six months. Importantly, potential participants must meet a range of detailed criteria relating to their medical history.
What are participants asked to do?
Participants are asked to attend an appointment to discuss the study in more detail and complete the informed consent process. They will then attend an initial research appointment and four further follow-up research appointments over two years at a local participating clinic. Clinic visits will involve the collection of demographic and health information, plus blood samples.
We want to hear your STORY– join a new study into eating disorders
We are trying to find out what characterises earlier and later stages of eating disorders, how symptoms change over time and what may help or hinder recovery. This information will allow us to develop and deliver more personalised and effective interventions tailored to the illness and recovery stages of young people with eating disorders.
Led by the University of Edinburgh and King’s College London, this study is open to people aged 16-25, who have an eating disorder or think they may have one. Young people who have no history of an eating disorder or other major mental health disorders may also be invited to take part in a control group.
Anyone interested will be asked to complete a brief screening questionnaire to confirm eligibility for the study. If you are enrolled, you will complete online assessments on your computer every few months over a year. You will download two apps onto your smartphone or a study smartphone provided and regularly complete short questionnaires. You may also wear a smart ring for 12 months to measure your heart rate and sleep, if you feel comfortable to do so.
You will be paid up to £175 for your participation and may receive a smartphone from us, as well as a picture of your brain. You cannot take part in STORY if you:
-
live outside the UK
-
have insufficient knowledge of English to complete study assessments
-
have a severe learning disability or any major medical disease which might impact your ability to participate in normal daily activities (e.g. due to hospitalisations).
For more information, watch the video below, visit the Edify website or contact the study team at STORY
Advertisement for the recruitment of volunteers for study REC reference: 23/PR/0927 (IRAS ID:325803), approved by the London - Bloomsbury Research Ethics Committee. This project contributes to the college’s role in conducting research, and teaching research methods.
The study co-ordinator is Deanna Rex.
Study deadline: 31 August 2025
GLAD
Genetic Links to Anxiety and Depression
Depression and anxiety disorders are the most common psychiatric disorders worldwide. This study aims to recruit thousands of people aged 16 or over diagnosed with, or being treated for, anxiety and depression to improve our understanding of the genetic risk factors behind these disorders.
The study will also include core mental health measures and some basic demographic and clinical data to assess the impact of environmental factors that may interact with genetic risk factors to produce these disorders.
People who consent to take part will be asked to complete some questionnaires and provide a saliva sample which can be analysed and added to the National Institute for Health and Care Research’s Mental Health BioResource. Participants will also be asked to give permission to the study team to access their medical record.
National Centre for Mental Health
Researchers at the National Centre for Mental Health (NCMH) are working to find out more about the causes of mental health problems. In particular, the study aims to understand more about how life experiences impact on maternal wellbeing and mental health during pregnancy and postnatally. The research aims to improve diagnosis and treatments of mental health problems.
The study is currently open to all perinatal mental health service users, and participants will be asked to provide basic information about themselves, their mental health, wellbeing and past experiences, as well as their experiences relating to COVID-19. The study team will also ask for permission to make contact 6-12 months following registration to ask about changes in their physical or mental health.
PPiP2: Prevalence of Pathogenic Antibodies in Psychosis
Research suggests that a small but significant proportion of people who experience symptoms of psychosis may, in fact, have a problem with their immune system – an autoimmune disorder. PPiP2 aims to see how many people with psychosis may have this specific problem with their immune system by carrying out a simple blood test for specific antibodies. If a problem with the immune system is found, participants may be eligible to take part in a study called SINAPPS2 which aims to test a new kind of treatment for this group.
This study is open to people experiencing symptoms of acute psychosis. Participants must be supported by Dorset HealthCare mental health services and meet criteria relating to their medical history.
Participants are invited to take part and complete a process of informed consent. Once a person consents, blood will be collected in the most convenient way for the participant – either concurrently with a planned blood draw, by inpatient staff or by research and development staff in a clinic or at the person’s home.
Eating Disorder Genetics Initiative (EDGI)
If you have experienced symptoms of any eating disorder, such as, excessive exercise, skipping meals, or using diet pills to lose weight, you may be eligible to join EDGI_UK. Sign up today at edgiuk.org!

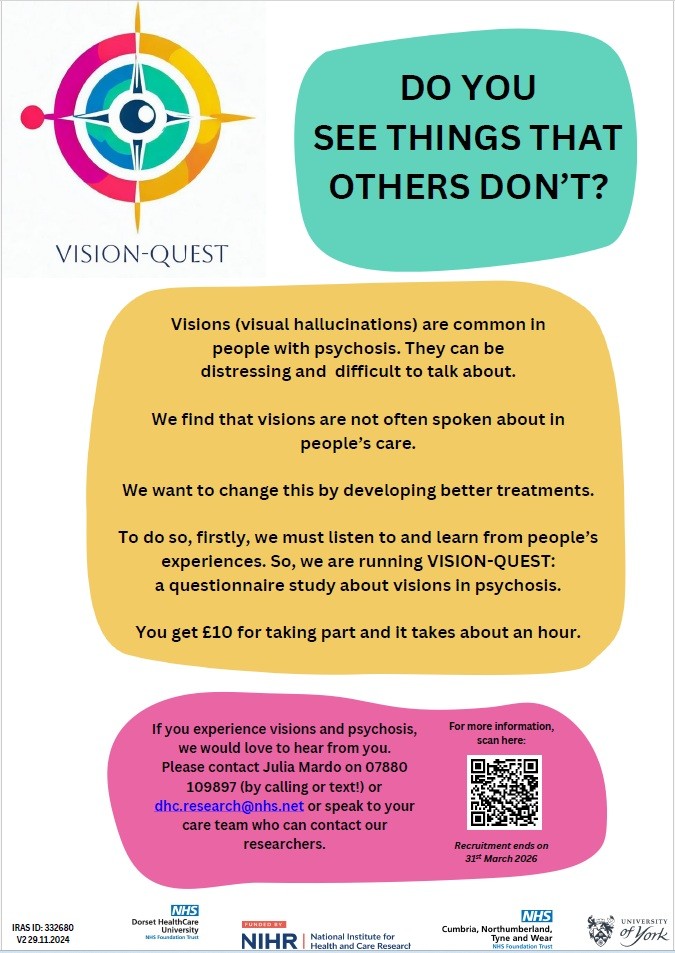
VISION-QUEST
The Weymouth Research Hub offers people in Weymouth, Portland and across West Dorset the chance to take part in vital, life-saving clinical trials.
Set up in the refurbished Linden Unit at Westhaven Hospital in Radipole Lane, Weymouth, the hub is a joint venture between Dorset HealthCare and Dorset County Hospital, with on-going support from the National Institute for Health and Care Research (NIHR) Wessex. Since its launch in 2023, volunteers have taken part in research into vaccines for COVID-19, shingles, norovirus, flu and more.
It's part of a south coast network of hubs – also including Southampton, Bournemouth and Portsmouth – set up by NIHR Wessex which work in collaboration with the NIHR Clinical Research Facility in Southampton. These centres played a frontline role during the COVID-19 pandemic in helping with the development of new vaccines. Thousands of people across the south came forward to volunteer, and played a vital role in helping to establish the national vaccination programme.
The NIHR Applied Research Collaboration (ARC) Wessex conducts applied health research with partners in the health and care sector, alongside patients and members of the public. Find out more and learn how you can get involved.
The Wessex ResearchLine is an online search tool designed to help users easily identify and contact clinical research studies running in the Wessex area.
Register your interest in participating in Dementia research.
Dorset County Hospital Research
Working in collaboration with Dorset County Hospital in research across the county.
UK Standards for Public Involvement - The UK Standards (google.com)